Physical Therapy with an External Fixator
Proven, Innovative Treatment for Your Child With a Limb Length Discrepancy
When an external fixator (EXFIX) is used to help treat your child's limb length discrepancy, physical therapy is essential in ensuring a successful outcome for your child. Physical therapy combined with an EXFIX can help create the best quality of life for your child.
During limb lengthening surgery, the process begins with an osteotomy, during which a skilled Shriners Children's orthopedic surgeon cuts the bone to be lengthened. The surgeon then stabilizes the limb using one of several different external fixation devices, called frames. The device has small rods, called pins, that go through the skin and into the bone.
This treatment is most commonly used on legs, but in some circumstances it can be done on arms as well.
Children with limb length inequalities, along with their families and caregivers, can look forward to a family-centered, multidisciplinary approach to their care at Shriners Children’s. Each treatment plan is individualized to the child’s and family’s specific goals and needs.
Our patients and their families are supported by our own Shriners “family,” our team of skilled, caring, and dedicated surgeons, nurses, orthotists and physical, occupational, and child-life therapists, throughout the continuum of care, and conveniently, all under the same roof.
Custom Treatment Plan Designed Specifically for Your Child
Shriners Children’s understands there is no “one size fits all" solution when it comes to specialized pediatric care.
Your child’s surgeon will work closely with you and the care team to create the best treatment plan to help your child reach his or her goals, and to meet your needs as a family. If a surgical lengthening is recommended, your surgeon will advise whether a lengthening with an external fixator, or with an Ellipse self-lengthening nail, would be the safest and most effective option for your child.
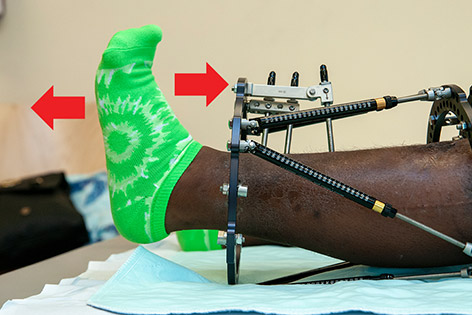
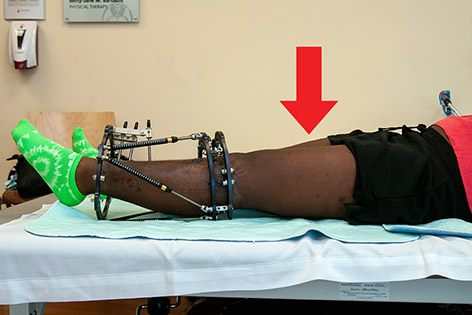
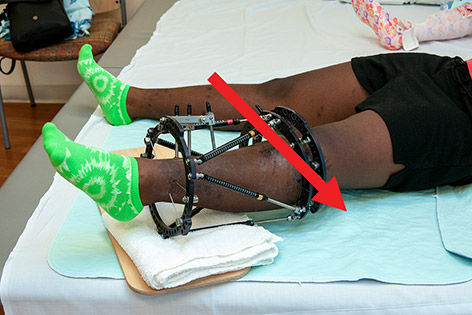
During surgery to lengthen a bone with an external fixator, the surgeon places an external fixator composed of metal rings and adjustable bars, called struts, to allow the gradual lengthening of the limb at the site where the bone has been cut, called an osteotomy or corticotomy. With an external fixator, the rings remain outside of the leg, and the caregiver assists with the lengthening process by turning the struts according to a specific schedule each day.
During surgery to lengthen a bone with a self-lengthening nail, the surgeon places the self-lengthening nail into the bone, and secures it with screws at each end of the nail. With an Ellipse nail, the nail and screws remain completely inside the leg, and the parent or guardian assists with the lengthening process by using an external magnetic device according to a specific schedule each day.
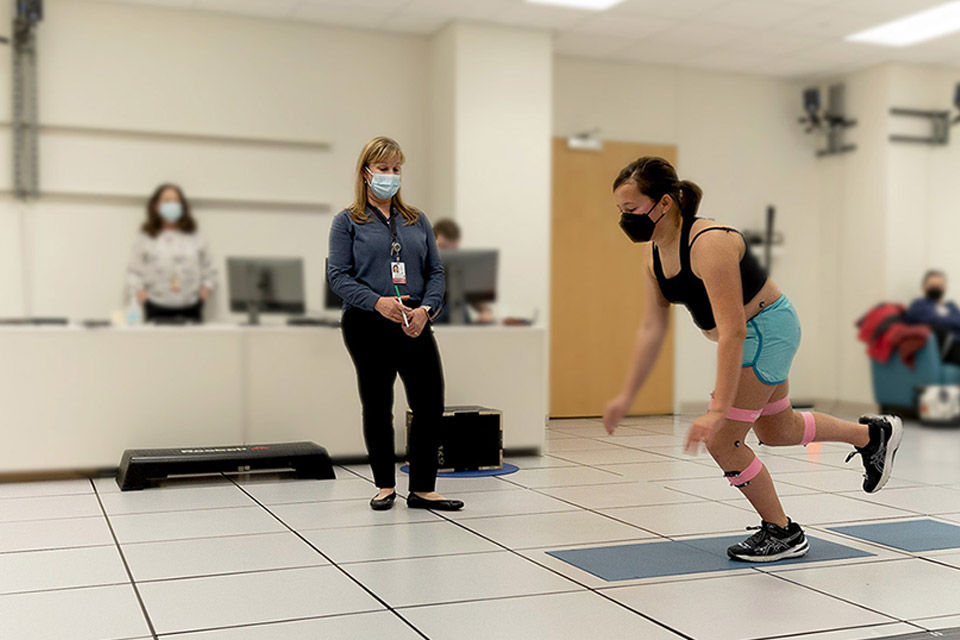
Personalized Physical and Occupational Therapy
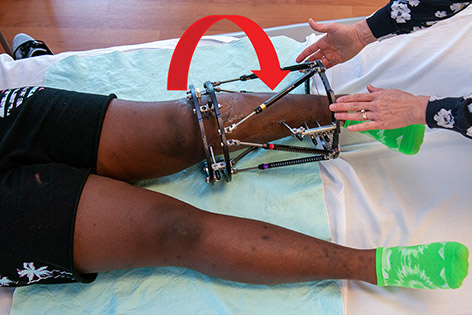
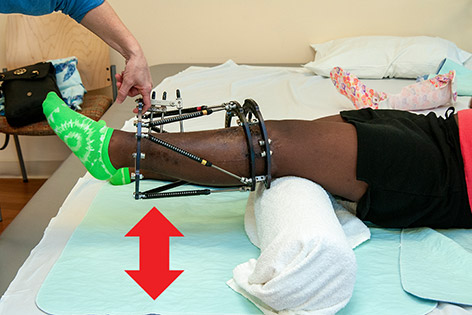
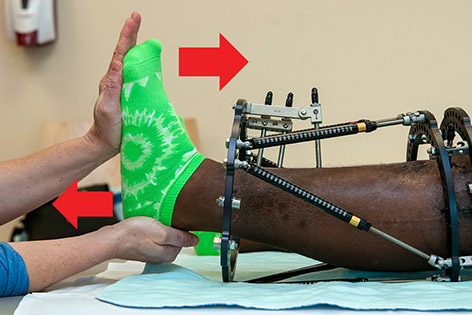
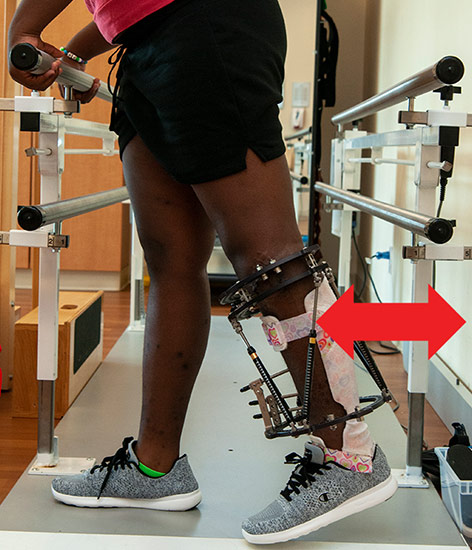
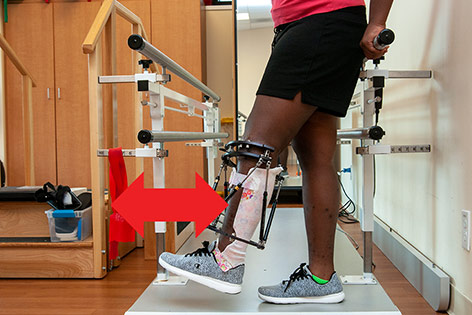
An individually designed physical therapy (PT) or occupational therapy (OT) treatment program is a critical component of any successful limb lengthening. You will most likely meet your physical therapist prior to surgery and may be given an exercise program at that time to prepare your child for the lengthening procedure. Each child’s course of therapy will include specific exercises to help stretch muscles and joints and to maximize strength as the limb is lengthened, along with functional activities to improve ease of movement and promote independent mobility and activities of daily living.
Outpatient PT or OT treatments and daily home exercise programs are prescribed while the limb is being lengthened, and continue through a subsequent period of bone healing and rehabilitation, which may continue for a total of six to 12 months on average. Some children will also benefit from a PT or OT exercise program to improve strength and mobility even before surgery, and will be provided with the necessary instruction and recommendations during a preoperative outpatient clinic appointment.
Family Participation in After-Care
Consistent, daily parent or guardian participation in each child’s after-surgery care is crucial to achieving a successful outcome. Parents or guardians participate in the following ways:
- Carefully adhering to the daily lengthening schedule for an external fixator or Ellipse self-lengthening nail
- Assisting your child with a twice daily home physical or occupational therapy exercise program to improve strength and range of motion in the limb being lengthened
- Ensuring your child’s adherence to activity guidelines or restrictions to either promote bone growth or to protect a bone as instructed
- Attending all postoperative clinic appointments with your surgeon, as scheduled
- Attending all postoperative physical or occupational therapy appointments, as scheduled
Shriners Children’s Is Here for You
Children with a more significant limb length discrepancy may require more than one lengthening procedure in order to equalize the limb lengths as much as possible. Whatever your child’s treatment plan, our Shriners Children’s specialized care team, our Shriners family, is here to guide and support you through every step of your journey.
Specific treatments and services may vary by location. Please contact a specific location for more information.
External Fixator Physical Therapy Instructions
The care, support and devotion Marie Eva received from Shriners Children's was never interrupted.